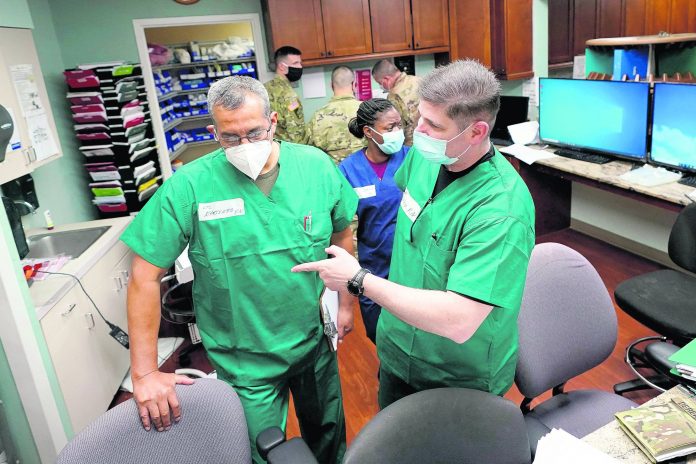
A fast-rising tide of new coronavirus cases is flooding emergency rooms in parts of the United States, with some patients moved into hallways and nurses working extra shifts to keep up with the surge.
Patients struggling to breathe are being placed on ventilators in emergency wards since intensive care units are full, officials say, and the near-constant care they require is overtaxing workers who also are treating more typical ER cases like chest pains, infections, and fractures.
In Texas, Dr. Alison Haddock of the Baylor College of Medicine said the current situation is worse than after Hurricane Harvey, which swamped Houston with floodwaters in 2017. The state reported a new daily record for virus deaths Friday and more than 10,000 confirmed cases for the fourth consecutive day.
“I’ve never seen anything like this COVID surge,” said Haddock, who has worked in emergency rooms since 2007. “We’re doing our best, but we’re not an ICU.”
Patients are waiting “hours and hours” to get admitted, she said, and the least sick people are lying in beds in halls to make room for most seriously ill.
Around Seattle, which was the nation’s first hot spot for the virus that causes COVID-19, a new wave of patients is showing up at emergency departments, said nurse Mike Hastings.
“What’s really frustrating from my side of it is when a patient comes into the emergency department, and is not really having symptoms of COVID, but they feel like they need that testing,” said Hastings, who works at an area hospital and is president of the Emergency Nurses Association. “Sometimes we’re not able to test them because we don’t have enough test supplies, so we’re only testing a certain set of patients.”
In Florida, another state that is seeing surging case numbers, hospitals say they are in desperate need of remdesivir — a medication that has been shown to shorten average hospitalization times — to treat the coronavirus patients who are filling up beds. In response, Gov. Ron DeSantis announced 30,000 vials of the drug were being shipped to the state — enough to treat about 5,000 patients.
On Saturday, Florida reported more than 10,200 new cases of the virus and 90 additional deaths, while Missouri recorded a pandemic-high 958 new cases in one day. Arizona, which conducts periodic reviews of death certificates, reclassified 106 deaths as having been from COVID-19, bringing the number of fatalities reported Saturday to 147.
Confirmed coronavirus cases around the world have surpassed 14 million, and deaths rose above 600,000, according to a tally from Johns Hopkins University. On Saturday, the World Health Organization, which also tracks the virus, reported a single-day record of new infections — over 259,000 worldwide — for the second day in a row. The true toll of the pandemic is thought to be even higher, in part because of shortages in testing and shortcomings in data collection.
The United States, Brazil and India top the list of cases, and South Africa — with more than 350,000 cases, roughly half of all confirmed infections in Africa — entered the top five this weekend.
In the United States, where infections are soaring in many Sunbelt states, Megan Jehn, associate professor of epidemiology at Arizona State Universtiy in Tempe, said it’s important to monitor emergency room visits since increases there can signal that the virus is spreading more rapidly.
But it’s difficult to get a complete picture of how emergency rooms are faring in many places. In Arizona, one of the few states that reports data on visits to the emergency room by people with confirmed or suspected COVID-19 symptoms, numbers started to spike in early June and peaked earlier this month. More than 2,000 people went to an ER with coronavirus symptoms on a single day, July 7.
On Friday, COVID-19-related hospitalization figures for Arizona were near but below recent records set after the state became a national hot spot.
Dr. Robert Hancock, who works at multiple hospitals in Texas and Oklahoma and serves as president of the Texas College of Emergency Physicians, said some Texas emergency rooms are facing backups of patients awaiting ICU beds. And many of them are on ventilators, meaning they require more attention than other patients.
“Unfortunately, because of the increased demand for personnel, there typically isn’t anybody free to come down to the ER to help a lot of times from a nursing standpoint,” he said.
Burnout could await these health workers, as it did some in New York City, when it was the epicenter of the nation’s outbreak in the spring.
Emergency room doctors and nurses were caught off guard by the relentless stream of severely sick patients during shifts that often lasted 12 hours, said Dr. Bernard P. Chang of New York-Presbyterian/Columbia University Medical Center.
“You were on high alert the whole shift,” Chang said. “It was a brutal, sustained battle.”